 |
 |
 Acupuncture Course Acupuncture Course |
 |
 |
|
|
 |
 Herbal Medicine Course Herbal Medicine Course |
 |
 |
|
|
 |
| About |
 |
 |
|
|
|
| About Course Chariman |
Introduction of course chairman: Tsun-Nin Lee, M.D
Dr. Lee's Philosophy of Traditional Chinese Medicine (TCM) -- Acupuncture and Herbal Medicine
Graduates' Comments on Dr. Lee
Sample Publications of Dr. Lee
|
MEDICAL HYPOTHESES VOL. 3 No. 3 MAY - JUNE 1977
THALAMIC NEURON THEORY: A HYPOTHESIS CONCERNING PAIN AND ACUPUNCTURE
Summary
Introduction
The Thalamic Neuron Theory (TNT) Part I
The Establishment Of Chronic Pain
Trigger Points And Basic Acupuncture
Accepted Medical Measures For The Treatment Of Pain
Thalamic Neuron Theory Part II
Acupuncture In General And The Expanded Thalamic Neuron Theory
Acupuncture Analgesia And The Tnt
Discussion
References
SUMMARY
A new theory is proposed to explain various pain phenomena hitherto unexplainable. It is hypothesized that neurons in the thalamic region are responsible for the generation of most pain, particularly in chronic pain states. It is also hypothesized that the thalamic neurons are organized according to a master scheme representing a homunculus in the fetal position. Various painful conditions and the treatments of them including the trigger points phenomena, neurosurgical techniques, acupuncture and acupuncture anesthesia can be explained on this basis.
INTRODUCTION
Despite many advances, the management of chronic pain remains problematical mainly because the neurophysiological mechanisms responsible for such pain are poorly understood. The recent renewed interest in the ancient Chinese healing science of acupuncture has thrown the currently prevailing pain theories into further disarray as the bulk of the acupuncture phenomena remain inexplicable by such theories. A new hypothesis is therefore required. Ideally such a hypothesis should provide a sound physiological explanation for all painful states. It should account for the relative efficacy of various therapeutic techniques including neurodestructive surgery and neuromodulation methods such as acupuncture in the treatment of chronic pain, as well as for acupuncture-induced surgical analgesia.
THE THALAMIC NEURON THEORY (TNT) PART I
Although the central pain mechanism as in phantom limb pain is a well recognized entity, the possibility that ALL chronic pain states are predominantly central in origin has not been seriously considered. Too much emphasis has perhaps been placed on the pain generating capacity of the peripheral neurons and those at the spinal cord level. By merely shifting the emphasis from the periphery to the thalamus as a source of chronic pain, many observations on the phenomena of pain may be more easily explained. Basically, the hypothesis consists of the following assumptions:
The intermediate neurons of the neural axis between the periphery and the sensory cortex are capable of not only relaying sensory impulses from the peripheral receptors, but also of autonomy under certain conditions. They can become hyperexcitable and, independent of the peripheral neurons, can discharge afferent neural impulses of their own which are appreciated consciously as pain.
Normal sensory inputs, such as tactile stimuli, may assume the characteristics of painful impulses after passing through abnormally hyperexcitable intermediate neurons.
Among the neurons at different levels of the neural axis of pain conduction, the thalamic neurons are the most liable to become autonomous and to develop a state of sustained hyperexcitability. They are the prime source of pain in the majority of if not in all chronic painful states. Other intermediate neurons such as those at the spinal cord level play only minor roles by comparison.
Repeated stimuli reaching the thalamic neurons can adjust their degrees of excitability upward or downward depending on the nature of the stimuli and the state of excitability prior to stimulation. Generally, the degree of excitability wil be normalized, ie, the same stiumuli can cause hyperxcitable neurons to becom less excitable while hypoexcitable ones more excitable
THE ESTABLISHMENT OF CHRONIC PAIN
Generally speaking, the most common cause of chronic pain is trauma, which may occur either abruptly or insidiously. In the case of acute injury, the entire neuro-axis involved in the transmission of pain is activated. But occasionally long after the original injury has healed, pain persists even in the absence of peripheral noxious stimuli, as in causalgia resulting from high velocity missiles (1) where 25% of the patients still complain of pain a year after injury (2). The thalamic neuron theory resolves this problem by considering the source of pain to be now resident in a specific group of neurons in the thalamus representing the painful region of the body. The barrage of neuronal discharges from the peripheral neurons at the time of traumatic injury is of such an explosive nature that it has activated these thalamic neurons to a sustained hyperexcitable state. After the hyperexcitable state is attained, ordinarily innocuous stimulation such as digital pressure applied to the area in question is now tran smitted to and modified by the hyperexcitable thalamic neurons into pain. In addition, the abnormal thalamic neurons can spontaneously discharge excessively even without provocation from the periphery. As far as the patient is concerned, he has no way of knowing that the pain originates from the thalamus: the previously injured part is both painful and sensitive to touch so that the pain seems to have arisen from the former site of injury.
Frequently, the chronic pain phase does not set in until after a lag period of days or even weeks has elapsed since the acute phase, as often is the case with the so called whiplash injuries involving the neck and back. So it appears that the alteration of excitability of the thalamic neurons may be mediated by a series of cellular biochemical events initiated by the bombardment of neural impulses on the thalamic neurons from the periphery at the time of injury. The latent period may be due to slow rate-limiting steps in the chain of biochemical reactions which eventually lead to hyperexcitability.
To extrapolate the hypothesis, any peripheral pain severe or prolonged enough may produce chronic pain by readjusting the sensitivity of the thalamic neurons upward. For example, while the dorsal ganglion is definitely implicated in the pathogenesis of herpes zoster, postherpetic neuralgia, on the other hand, may actually be the sustained activation of those thalamic neurons that correspond to the involved neural segment as the result of the constant firing of painful stimuli onto them by the peripheral nerve during the acute phase. In the case of phantom limb pain, severe pain in the amputated extremity prior to operation is frequently present and may have already initiated the chronic pain process, or the afferent pain impulses from the amputation itself may stimulate the thalamic neurons intensely enough to set up the chronic pain in a thalamic focus although the sensation of pain never reaches consciousness during the procedure under general anesthesia. A third possibility is that post-operative pain may be strong enough to evoke the same response from the thalamic neurons.
Chronic pain can also be set up insidiously as a result of the cumulative effect of repetitious micro-trauma as in various myofascial syndromes (3,4). The epicondylitis in a tennis professional (5), the painful shoulder of a machine operator and the painful wrists of a butcher all stem from a common denominator: repeated action and trauma to the same neuromuscular elements. From the standpoint of the Thalamic Neuron Theory (TNT) each minor ache excites the corresponding neurons in the thalamus while prolonged, repeated stimulation has a tendency to habituate these neurons to a constantly hyperexcitable state and hence a state of chronic pain. Once the hyperexcitable state has stabilized, the removal of the original causative factors, namely the cessation of the particular neuromuscular activity, will not mitigate the pain though this may prevent further worsening of the condition.
Pain in osteoarthritis may well be derived from similar mechanisms. Age, trauma, and occupation which are generally considered to be the major contributing factors in the development of osteoarthritis all point to chronic repetitious trauma to the involved joints. The hypertrophic osseous changes at the joints usually occur at the points of maximum stress at or near the attachments of tendons. This is a matter of bone growth in response to the stress force and the degree of trophic changes is proportional to the amount of stress and not necessarily the amount of trauma. Consequently, the severity of pain in osteoarthritis frequently does not parallel the degree of trophic changes in the joints. In other words, the hypertrophic change is merely a concurrent finding and not in itself a cause of pain, contrary to current beliefs. Hence, it is possible to relieve osteoarthritic pain with acupuncture which subdues the hyperexcitable thalamic focus representing the involved joints, even though the structural deformities in the joints remain the same.
Other painful states unrelated to trauma but which seem spontaneous or infectious in origin, such as tic douloureux, rheumatoid arthritis, myalgia in viral syndromes, etc., may similarly involve the thalamic neurons. This ultimate thalamic involvement in a wide variety of painful conditions may indeed be the basis for the versatility of acupuncture in treating many painful states with markedly different etiologies. The mechanism of acupuncture will be discussed in the following sections
TRIGGER POINTS AND BASIC ACUPUNCTURE
A trigger point by definition is a locus on the body surface, which upon stimulation will trigger pain in an area adjacent to the locus itself or at some distance away (3,6). Trigger points are present in many chronic as well as acute painful states. Triggering phenomena in trigeminal neuralgia, chronic low back syndrome, and myofascial syndromes are familiar ones. The injection of these points with local anesthetics or saline has been proved useful in the treatment of neuromuscular pains. Although trigger points may occur at any location, some seem to occur frequently at definitive locations with great consistency. A comparison of the frequently occurring trigger points with the classical acupuncture points shows a remarkable coincidence and the areas of referred pain elicited by stimulating such points follow the distribution of the acupuncture meridians (7).
From the standpoint of the TNT, the trigger points or acupuncture points are represented in the thalamus by specific groups of neurons. In other words, the sensory nerve fibers that supply the trigger point in the periphery feed into neural pathways that eventually project into such neuronal groups in the thalamus. In acute pain, the group of thalamic neurons corresponding to the painful part of the body over-fires as they are bombarded by the afferent impulses from the peripheral pain receptors, but here the thalamic neurons are passive, functioning merely as a receptor and relaying apparatus. In chronic pain, however, the thalamic neurons are independently active in a habituated state of hyperexcitability and become the origin of pain impulses themselves. But neither the physician nor the patient can distinguish clinically from which level of the neural axis does the pain originate because the subjective sensation is the same and the peripheral part of the body remains objectively tender to palpation in both situations.
The anatomical distribution of pain elicited by stimulating various trigger points and the phenomena of referred pain cannot always be adequately explained or predicted by the peripheral segmental nervous system. Using the thalamic neuron model, however, one can visualize the stimulation of a trigger point to be equivalent to stimulating the corresponding hyperexcitable thalamic neurons, which will also excite contiguous thalamic neurons that represent the referred pain area. So the pattern of pain radiation from trigger point stimulation reflects a central phenomenon at the thalamic level rather than one at the segmental level.
One of the basic principles in traditional Chinese acupuncture is "let pain be the guidance for the needle". The principle was recorded as early as 400 B.C. (8). What it means is that painful or tender spots or trigger points, regardless of whether they are well-established acupuncture loci or nonspecific reactive points, should be punctured in administering acupuncture therapy. The principle, simple as it may be, ensures that the acupuncture stimulus reaches the corresponding specific focus of excited thalamic neurons, which upon stimulation, tends to normalize or decrease in excitability, leading to a reduction in pain. In reality, pain relief accomplished with a single treatment is often temporary. Therefore, the second basic acupuncture principle is to repeat the treatment at closely spaced intervals [every day or every other day). By so doing, the pain relief after each additional treatment tends to be more sustained and permanent. From these observations the hyperexcitable thalamic neurons seem to be capable of learning from repeated stimulations to adjust their excitability to the normal level. This process of normalization through habituation appears to be just the reverse of the setting up of chronic pain from a series of microtraumas.
Massaging or injecting the trigger points with saline achieves therapeutic results in much the same way. Again, clinical success hinges upon repetition of the same procedures. There is, however, one trigger point phenomenon which remains to be accounted for, namely the therapeutic success in treating pain by injecting local anesthetics into the trigger points, as there is no sensory input to stimulate the thalamic neurons in this case. Paradoxically, however, the absolute lack of sensory input itself can be construed by the thalamic neurons as a form of stimulation. Under normal conditions, the peripheral receptor has a low rate of spontaneous firing which may have assisted or potentiated the maintenance of hyperexcitable state of the neurons in the thalamus. The sudden interruption of otherwise constantly present afferent impulses impinging on the thalamic neurons is, in fact a stimulation to these neurons. Such a stimulation has a tendency to normalize the hyperexcitable state just like the other benign non-specific stimulations produced by acupuncture, saline injection and digital massage. The duration of stimulation is the same as the duration of local anesthetic effect. Quite often, the resulting analgesic effect from blocking the trigger points lasts much longer than the action of the local anesthetic itself (3). This is not surprising as the reduced level of pain from acupuncture also lasts much longer than the duration of the treatment. From the viewpoint of the TNT the excitability of the thalamic neurons, once lowered by nonspecific benign afferent stimulations, will remain lowered long after the original stimulation has dissipated. It appears that the crucial role of these stimulations is to initiate a chain of cellular biochemical events that tend to normalize the degree of excitability of these nerve cells. At times pain relief from even repeated acupuncture or trigger point injections may not be obtained until a variable lag period of hours, days or weeks has elapsed, indicating the normalizing process may involve a series of slow biochemical reactions. This lag period of the waning of pain after treatment is parallel to the latent period in the onset of pain after a traumatic episode, only they are opposite in directions. Occasionally, after either acupuncture treatment or trigger point injection, pain will exacerbate before it will get better. One possible mechanism for this kind of reactive phase or transient rebound phenomenon may involve the sudden release of excessive amounts of neurotransmitters from the hyperexcitable neurons causing a transient period of increased pain. Once the hyperexcitable thalamic neurons are rid of their overabundant supply of neurotransmitters, their excitability is restored to normal with a concomitant reduction of pain.
ACCEPTED MEDICAL MEASURES FOR THE TREATMENT OF PAIN
In modern medicine, a number of operative techniques have been divised to intercept the pathway of pain or change the response to it by destroying nervous tissues. Among them are thalamic and suprathalamic procedures such as thalamotomy, cingulotomy and lobotomy, and infrathalamic techniques including peripheral neurectomy, cordotomy, rhizotomy, sympathectomy and medullar tractotomy.
Cingulotomy and frontal lobotomy do not actually interrupt the projection of painful impulses to the sensory cortex, nor change the threshold of pain: they merely alter the subjective reaction to pain. Variable success with thalamotomy has been obtained by different investigators (9,10,11) or the same investigators at different times (11,11, 13). The most recent report by Fairman and Llavallol (11) indicated a 70% rate of success in relieving severe chronic pain in 165 cancer patients and the degree of relief lasted the entire period of survival. The infrathalamic procedures, however, are marked by a low success rate with a high rate of recurrence (14,15). If the postulations of the TNT are true, one would expect a more effective control of chronic pain by using neurodestructive techniques at the thalamic level since they are disrupting pain generation in the source. At the present time, it is difficult to evaluate the long term effect of thalamotomy as the patients do not survive long enough. Besides, the thalamus itself is a complex and sizable structure, so sectioning or destroying part of it does not necessarily mean destruction of pain generating thalamic neurons. Therefore, presently available neurosurgical data can neither refute nor confirm the thalamic neuron theory. One may argue however, that since the source of pain is assumed to be contained in the thalamic structures, cutting the neuroaxis below the thalamus should not be effective in relieving the pain at all. But in reality a small percentage of patients undergoing infrathalamic procedures do obtain permanent pain relief and this phenomenon must be accounted for.
The sectioning of a neural conduit is more or less equivalent to a nerve block with a local anesthetic with infinite duration of action. The prolonged absence of afferent impulses acts as a single powerful stimulus to the hyperexcitable thalamic neurons which are thus pushed
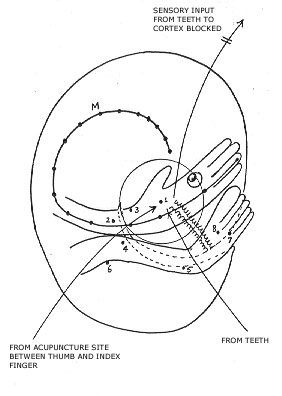
Figure 1.An hypothetical embryonic posture of the thalamic homuncu-lus. The curved line M travailing from the head to the hand represents a chain of thalamic neurons equivalent to an acupuncture meridians. The small dots along its course represent neuronal aggregates corresponding to acupuncture points in the periphery. This special spatial arrangement of neurons within the thalamic homunculus can explain the effects of acupuncture points on regions of the body that seem to bear no segmental relationship with them. See Table I for details. The Con-valley point between the thumb and index finger shares with the teeth the same group of thalamic neurons in afferent transmission. Acupuncture stimulation at the Con-valley point can therefore block the transmission of pain from dental operations.
Figure 2.Nerve fibers representing different sensory modalities tend to project to different nuclei or structures in the thalamus and there may be so much overlapping that the homunculi for different modalities cannot be easily isolated anatomically. In addition the individual homunculi may have markedly different postures and spatial arrangements of their con-stituent neurons, but as long as they are connected to one another equivalently, namely, head to head, toe to toe, knee to knee, etc. and one of them, the controlling homunculus is arranged according to the embryonic plan (H), then they still can behave collectively as a com-posite sensory homunculus in the shape of an embryo. A possible can-didate for the embryonically postured homunculus is the ancient para-fasicular nucleus which situates in the medial thalamus close to the third ventricle. It is also possible that the embryo like structure is actually within the hypothalamus and then connects with the thalamic homnculi. (H) may be quite minute in size.
towards normalization. But the chronically hyperexcitable neurons are much more likely be normalized by habitu-ation through REPEATED stimulations, whereas cutting the neural axis infrathalamically is tantamount to a SINGULAR stimulation, which is powerful though insufficient in the majority of cases to permanently normalize the hyperexcitable thalamic neurons. Similarly, one single acupuncture treatment can induce permanent relief in only a small percentage of patients, and that is why a series of treatments is usually necessary. Even when excellent pain relief is obtained with a single acupuncture treatment, it is still important to repeat the treatment several more times to forestall future recurrence. The infrathalamic neurodestructive techniques such as rhizotomy are like a good single acupuncture treatment that can never be repeated, and the recurrence rate is high (16,17). Just as an episode of severe acute pain will set up chronic pain in only a small number of patients, one good treatment can remove it permanently in an equally small number. The occasional success of the neural destructive surgical techniques has misled investigators in the past into overemphasizing the roles of the peripheral segment of the pain pathway in the generation of pain and persisting in techniques of meager value associated with frequent complications and morbidity.
THALAMIC NEURON THEORY PART II
Although a shift in emphasis from the periphery to the thalamus in considering the mechanism of generation of pain provides an answer to some of the unresolved clinical questions as delineated above, the TNT in its present form is still inadequate to explain the bulk of analgesic effects of acupuncture since the punctured sites often seem to bear no anatomical relationship to the painful area. A refinement of the Thalamic Neuron Theory is therefore necessary in order to take these phenomena into account. The Thalamic Neuron Theory is expanded as follows.
Table 1: Efficacy of Acupuncture Points in terms of central connection in Thalamic Homunculus.
Acupuncture Points
| Chinese Names |
English Equivalent |
Anatomical locations of Points |
Assigned number in Figure I |
Regions of body controlled and treatable by the
Points |
| Ho-Ku |
Con-Valley |
Web Space between thumb and finger |
1 |
face and mouth |
|
| Nei-Kuan |
Inner Fort |
2 inches proximal to wrist at center line of flexor surface |
2 |
heart and thorax |
|
| Lieh Ch'ueh |
Split Space |
1 inch proximal to styloid process of radius |
3 |
head and neck |
| Tsu-San-Li |
Leg-Three-Lanes |
1 inch distal and lateral to the tibial tuberosity |
4 |
abdomen |
| San Yin Chiao |
Tri-Yin Merger |
3 inches above the medial maleolus at posterior border
of tibia |
5 |
lower abdomen and pelvic region |
| Wie-Chung |
Fold Center |
Center of popliteal fossa |
6 |
back |
| Pai-Hui |
Grand Concourse |
vertex of head |
7 |
head and anal region |
| Nei-Ting |
Inner Court |
Between 2nd and 3rd toes |
8 |
teeth and feet |
-
Thalamic neurons involved in pain transmission
are themselves organized as a homunculus which may be contained in the
phylogenetically ancient parafasicular nucleus which is a pain receiving
center in the thalamus, or in several other thalamic or hypothalamic structures
as well.
-
The thalamic homunculus assumes the
shape and posture of a primitive embryo with its large head buried close
to its pelvic region and its large hands and feet crowded together in the
vicinity of the face (fig. 1).
-
Along the longitudinal axis of the homunculus
are chains of neurons which are functionally closely related and generally
behave in a concerted manner. These chains of neurons are equivalent to
the acupuncture meridians (fig. 1).
-
Along the meridian neuron chains are
functionally but not necessarily histologically discrete groups of neurons
which are more sensitive to stimulation and more exaggerated in functions
in reflecting the change of the state of excitability of the entire neuron
chain. These groups of neurons are equivalent to the classical acupuncture
points (fig. 1).
None of the above
postulations is in conflict with known facts of neuroanatomy or neurophysiology,
even though they are merely assumptions requiring experimental confirmation.
Hassler mapped out a homunculus in the sensory thalamus in man by observing
the unpleasant tingling effect in various parts of the body elicited by
stimulation of thalamic sites in the course of stereotaxic surgery (18).
However, he did not specifically demonstrate the embryonic posture of the
homunculus. But considering the limitation of the technique in outlining
a very small, highly complex three dimensional structure, the embryonic
posture cannot be ruled out. In view of the overall elipsoid shape of the
thalamic structure, the curled up embryonic shape is compact and economical
in space in terms of organization. An attempt is now made to decipher the
enigmatic nature of the analgesic effects of acupuncture using the above
hypothesis.
ACUPUNCTURE IN GENERAL AND THE EXPANDED THALAMIC NEURON THEORY
The fact that stimulation of an acupuncture point can subdue chronic pain in a totally unrelated neuroanatomical region is truely puzzling. Some acupuncture points are considered to be supremely important in treating pain in certain general areas of the body despite minimal or lack of segmental relationships (see Table I) (Fig. 1), which, however, does not rule out their relationships in the central nervous system, or more specifically, in the highly associative thalamic nuclei. Using the embryonic model of the thalamic homunculus it can be shown diagramatically that those neuronal groups representing such acupuncture points and the respective therapeutically responsive areas are in fact physically adjacent (Fig. 1). Based on this arrangement, the chronically hyperexcitable thalamic neurons corresponding to the pain-afflicted area can be normalized by stimulating the general vicinity of these neurons within the homunculus via acupuncture points which seem to bear no apparent segmental relaionship with the painful area in the periphery.
Based on the anatomy of the peripheral nervous system alone, it is difficult to visualize how a point on the vertex of the head can be used to reduce hemorrhoidal pain or how stimulating a locus between the second or third toe can subdue a toothache. Based on the second postulate of the expanded Thalamic Neuron Theory, however, the homunculus neurons representing the anal region are juxta-positioned to those representing the vertex of the head (Fig. 1). Similarly, the neurons of the foot lie in close proximity to those corresponding to the face.
The TNT also provides a physiological foundation for the acupuncture meridians which have so far defied scientific explanation because they cannot be demonstrated to exist on the body surface as anatomical entities. In accordance with the TNT, they will never be demonstrated in the periphery because they only exist in the thalamic homunculus as neuron chains. The so called flow of Chi (vital energy) along the meridians as described in classical Chinese medical literature is really equivalent to neural transmission along these neuronal chains. One can assume the propagation of neural impulses along each neuronal chain is a facilitated one. Functionally, a neuron chain in the homunculus acts as an integrated system. Therefore, if a group of neurons or a segment of a meridian chain become abnormally active as in chronic pain, the other neurons or segments along the same meridian chain are more likely to be affected. Such a hypothesis will explain the phenomena of referred pain or the pathways of pain radiation resulting from stimulating the trigger points. When a trigger point is stimulated, the corresponding hyperexcitable neurons in the thalamic homunculus will spread the excitation in the neighborhood and along the meridian neuronal chain, giving rise to the subjective sensation of pain spreading to the corresponding area in the periphery. Hence referred pain following the distribution of the meridians (7) is primarily a CNS event, or more specifically, a thalamic occurrence. The classical meridians marked on the body surface are merely the images of the meridian neuron chains in the thalamic homunculus and not anatomical entities in the periphery.
From a functional point of view, the neurons in the same meridian behave as though they were physically adjacent to each other due to facilitated transmission. This is a highly useful concept from the therapeutic point of view because a normalizing stimulation has the tendency to propagate along the meridian so it can calm abnormally excitable neurons even at considerable distance. This view is consistent with the classical acupuncture concept that stimulating acupuncture points in a meridian has the tendency of adjusting abnormality along its course.
Postulate 4 of the TNT assumes unequal activities and sensitivities of those neurons in the meridian chains. Aggregates of neurons in the homunculus corresponding to the acupuncture points are more responsive to afferent sensory stimulation and are also more influential on other neurons in the same meridian. When chronic pain is set up in a focus of the thalamic homunculus as a result of trauma, the neurons corresponding to the acupuncture points within this focus become more excitable than the other neighboring neurons so they also represent the trigger points. This explains why trigger points often coincide with acupuncture loci and occur at constant anatomical locations with such a high frequency. However, the point of maximum trauma such as muscular strain or tear does not usually occur at the acupuncture point, so in this case besides the activated acupuncture point there can also be other major trigger points known as reactive points, which have been discussed earlier. It is quite likely that whenever an injurious incident takes place within the circle of influence of an acupuncture locus, it can activate and convert the latter into a trigger point.
ACUPUNCTURE ANALGESIA AND THE TNT
There is a subtle but significant difference in the use of acupuncture to treat chronic pain and in the induction of surgical analgesia. In chronic pain, the source of pain originates from the thalamic focus. To take away this kind of pain it is necessary to install frequent repeated sessions of stimulation daily or on alternate days and therapeutic effects are often delayed. In acupuncture analgesia, on the other hand, the source of pain arises from the periphery, namely, the surgical field; the analgesic effect is immediate after a short period of induction with acupunctural stimulation; the analgesia thus effected is usually incomplete and of course, there can be no repeated sessions. In the chronic pain state, specific thalamic neurons are hyperactive prior to acupuncture stimulation whereas all the thalamic neurons are normoactive at the time of induction of acupuncture analgesia. In contrast to acupuncture therapy, acupuncture analgesia requires a high frequency of stimulation (generally over 100/minute) either by manual manipulation or electrical pulsation. In addition, continuous acupuncture stimulation of no less than 15 minutes is usually necessary to induce satisfactory analgesia.
Before applying the TNT to explain the phenomena of acupuncture analgesia, consider again the entire pathway of pain conduction. Pain impulses originating from the surgical field must traverse a number of synapses at various levels of the nervous system before they are consciously perceived. Now suppose one or more of these synapses is rendered inoperative, then the afferent impulses of the noxious stimuli will be interrupted and analgesia results. One way of accomplishing this end is to temporarily deplete or substantially reduce the amount of neurotransmitters available at the presynaptic terminals at one or more of these synapses. One of the important synapses is at the thalamic level. But due to the peculiar spatial arrangement of the thalamic sensory homunculus and the meridian neuron chains, these very same thalamic neurons representing the surgical field and those in the same vicinity within the thalamic homunculus are also connected to certain acupuncture points on the body surface which seem to be segmentally unrelated to the surgical field. By administering acupuncture stimulation at these loci at a rapid rate, the thalamic neurons are stimulated and will discharge accordingly, so it becomes possible to release neurotransmitters from the specific thalamic neurons much faster than their reuptake. Consequently the cumulative effect of repeated stimulations during the induction period is to deplete available neurotransmitter in the thalamic neurons representing the surgical field and thereby render selective synapses at this level ineffective so that specific analgesia can be accomplished. The inactivated thalamic synapses will curb the spread of painful impulses within the thalamus and thereby markedly reduce the total response to noxious stimuli arising from the surgical field. Moreover, further transmission to the cortical level may also be prevented so that emotional arousal to the residual pain can be dulled. As an example, acupuncture stimulation of the con-valley point between the thumb and index finger can inactivate thalamic synapses in a large area corresponding not only to the hand but also the face and mouth including the teeth. Therefore pain from dental operations can be sharply reduced and acupuncture analgesia is accomplished (Fig. 1). Continuous stimulation during surgery is used to maintain this low level of activity of the thalamic synapses. This hypothesized mechanism can also explain a period of several hours of post-operative analgesia as the depleted neurons will require several hours to replete their neurotransmitters from biosynthesis or other mechanisms. By the same reasoning synaptic blocking can also occur at the spinal cord level. In this case, the acupuncture points must be related to the surgical field segmentally since afferent impulses from the acupuncture locus will have to inactivate the intermediate neurons in the spinal cord which it shares with the surgical field. By combining the spinal cord blockade and the thalamic blockade, the transmission of operative pain can be subdued even more effectively for it is simultaneously weakened at two different levels of the transmitting pathway.
DISCUSSION
M. R. Delgado was successful in controlling chronic intractable pain in an automobile accident victim by repeatedly stimulating the head of the caudate nucleus and the septum through electrodes leading from a stimoceiver under the scalp. The patient was still pain free 2 years later after receiving only 2 months of repeated stimulation (19). It appears the brain is capable of learning to eliminate pain through repititous stimuli. Kandel was able to demonstrate the gill withdrawal reflex in Aplysia to tactile stimulus will cease after repeated identical stimulations (20), implying the animal can learn and remember with its simple abdominal ganglion by readjusting the sensitivity of certain specific neurons. Conditioned reflex, habituation, memory are processes of learning which all depend on a common denominator: the setting up of definitive neural circuits through repetitious input to the CNS: once established, they can be activated upon situational demands. The conduction of neural impulses along such circuits must be facilitated or the resistance to conduction of neural impulses is preferentially reduced. Individual neurons comprising any such neurological pathway must also undergo readjustment of their sensitivities to attain this goal. It follows therefore repeated sensory stimulations can result in a change in neuronal sensitivity in specific nerve cells. Consequently, it does not seem too unreasonable to assume the ability of the thalamic neurons to respond to repeated stimuli by readjusting their "painstats", namely, their sensitivities to sensory impulses and their excitabilities to produce pain.
From the evolutionary point of view, the capacity to benefit from past experience through the process of learning enables the organism to cope with its environment and enhances its chance of survival. Phylogenetical advancement is parallel to an ever increasing ability to learn. In the higher forms of animals the central nervous systems are so specialized in learning that they possess the inherent disadvantage of learning chronic pain as well. But since the survival value of such a nervous system far outweighs its deficiency, the entire system including its flaws has been preserved in the course of natural selection. Moreover, chronic pain is presumably of relatively rare occurrence in the animal kingdom and when it is present, it does not seriously affect survival or the propagation of the species.
Assuming the ability of the thalamic neurons to learn and habituate through repeated stimuli as hypothesized in the TNT, a few inferences may be drawn. All too often, effective means of pain control such as injection of steroids or local anesthetics into trigger points are given up because the relief is only temporary. The early withdrawal of this particular type of therapy is a direct result of the failure to recognize frequent consecutive treatments are necessary to habituate the hyperexcitable thalamic neurons into a normalized state permanently despite short term relief with each treatment initially. It can be predicted, therefore, by simply persisting in rendering these therapeutic modalities on a more frequent schedule (e.g. every other day) and for a much longer duration, the success rate in eliminating chronic pains by using these treatments alone will be improved considerably. By the same token, the preliminary test blocking of a trigeminal branch with anesthetic agents before neurectomy in the treatment of tic douloureux may indeed be a far superior therapeutic modality than the neurodestructive technique itself if the nerve block is repeated over and over again. Aside from the inevitable morbidity, all forms of neurodestructions are unsatisfactory in accomplishing long lasting relief because they do not provide the repetitious stimuli necessary to habituate or reset the neuronal painstat. Indeed, once the destruction of nervous tissue has occurred, a useful pathway for neuromodulation is permanently lost.
The thalamic neuron concept may have significant applications in the prevention of some forms of chronically disabling pain. For example, phantom limb pain may be prevented altogether by treating the limb pain not only with analgesics and narcotics but with nerve blocks before, during and after the surgical procedure to keep the barrage of pain impulses impinging upon the thalamic neurons to a minimum so as to avoid habituating them into a hyperexcitable state and the occurrence of phantom limb pain may perhaps be averted.
The presumed existence of a sensory homunculus in the thalamus as postulated here is not in conflict with presently known scientific facts. Inasmuch as the thalamus is the major stopover for the transmission all sensory modalities originating from different parts of the body, a homunculus or homunculi almost have to exist at this level simply from an intuitive point of view and indeed it does, as demonstrated by Hassler (18). The question is not whether a sensory homunculus exists but how many homunculi are there in the thalamus and how are they organized internally and among each other. Nerve fibers representing different sensory modalities such as pain, temperature, touch, vibratory sense, appear to project to different nuclei or structures in the thalamus, so there may be as many sensory homunculi as there are sensory modalities. Being a highly integrated system, the thalamus is rich in intrathalamic connections to assimilate the various pieces of sensory information and through such a network of association, the homunculi representing diverse sensory modalities converge into and behave collectively like a single multi-sensory homunculus (Fig. 2). This functional homunculus is the thalamic homunculus referred to in the expanded thalamic neuron theory and the basic architectural plan of such a homunculus is that of a primitive embryo. Through the integrative intrathalamic network, it may be possible to stimulate specific regions of one of the homunculi in order to affect equivalent regions of other homunculi. For instance, if the knee region of the proprioceptive homunculus is stimulated, it will in turn stimulate the knee region of the pain homunculus via intrathalamic connections and normalize the sensitivity of the neurons responsible for pain in the knee. Such an integrative mechanism can account for the fact that acupuncture, which may involve proprioceptive stimulation without any sensation of pain, and moxibustion which utilizes temperature as the modality of stimulation, can still have significant therapeutic effects on pain. Conversely, when certain parts of the homunculus representing one modality become abnormal, equivalent parts of other homunculi can also be affected adversely. For instance, when chronic pain is established in the leg, then the neurons in the leg of the pain homunculus are in a hyperexcitable state, which in turn can cause functional derangement in the leg regions of other homunculi, thereby causing concurrent burning, pins and needles, pulling or numbing sensations in the leg depending on which homunculuss or homunculi representing other sensory modalities are affected. Such mixed sensory characteristics associated with chronic pain are often encountered in clinical situations. The functional sensory homunculus can be visualized as a sum total of all the composite homunculi of various sensory modalities.
Based on these assumptions, it is now possible to explain why thalamotomy is not always effective in controlling chronic pain. First of all, sectioning of thalamic tracts or stereotaxic destruction of thalamic tissue may not involve the pain generating neurons directly and all it does is to accomplish more or less the same thing as the infrathalamic neurosurgical techniques by imparting a powerful stimulus to the hyperexcitable thalamic neurons to normalize by a sudden lack of sensory impulses. Thalamotomy can of course also curb the spread of neurotransmission within the thalamus and reduce the intensity of pain, while total elimination of it may still be quite difficult. Additionally, stereotaxic surgery of the thalamus is usually performed as a last resort to control intractable pain. By this time neurons in the other sensory homunculi corresponding to the painful area in the pain homunculus may have already been activated to abnormally excitable levels via the intrathalamic connections. As a result, they have a tendency to reactivate the original thalamic neurons for pain despite the fact that some of them may have been destroyed neurosurgically.
Finally, the embryonic posture of the sensory homunculus as hypothesized will require somewhat more elaborate theoretical consideration. Before presenting arguments in support of the viability of this concept, several well-known scientific facts need to be reviewed and considered.
-
The appearances of the fetuses of various animals at different levels of the phylogenetical scale are remarkably similar in the earliest stage of embryonic development. This is generally construed to be a strong evidence in support of the theory of evolution that all species have a common origin.
-
Phylogenetically, the thalamus is the oldest part of the brain and as a rule the more medial a thalamic structure is, the more ancient it is in the phylogenetical scale. Recently, Chang has demonstrated experimentally in albino rats and rabbits that pain sensitive neurons are distributed mainly on the parafascicular nucleus and the central lateral nucleus in the medial thalamus (21). The characteristic discharge of certain neurons in these nuclei in response to noxious stimuli can be inhibited by electrical needling of certain acupuncture points, suggesting that the afferent impulses from the acupuncture points have acted on the afferent impulses from the origin of pain within these structures so that the degree of pain becomes negligible (21).
-
The embryonic neural tissue controls the development of the nervous system as well as the somatic components.
If phylogenetical history is traced back far enough, it would be theoretically possible to find an organism whose adult from deviates little from the primitive embryo with none of the brain structures of higher animals except for a minute remnant of the oldest or most medial thalamic structures. This primordial "brain", however, still must represent the whole body of the simple primordial organism or organized as a homunculus. In this animal, its body and nervous system are both constructed according to the same blue print dictated by the genetic material. The CNS homunculus may indeed resemble the primordial organism so much that it can be viewed to contain the master plan for somatic development itself. Consequently, it is not surprising at all that this primitive brain, which may be somewhat equivalent to a small thalamic nucleus, is organized in the shape of an embryo. The primitive CNS may be primarily designed for the detection of noxious stimuli, the most important and oldest sensory modality necessary for survival. In the course of evolution, other modalities, such as temperature sense, light touch, vibratory sense and so on, developed and these more specialized structures or nuclei were added to the oldest brain to form the thalamus and remain in close association with it. Although the other sensory homunculi representing different modalities may not now resemble the embryonic plan in any way, the overall functional homunculus (sum total of all sensory homunculi) will still behave as if it is structured according to the embryonic plan, provided that the oldest nucleus follows the plan and at the same time intimately associates with other nuclei or structures.
The parafascicular nucleus may be in fact a derivative from, or closely related to, the primordial "brain". In order to prove a hypothesis of this kind, it is imperative to locate at least one structure in the paleothalamus that is organized in the shape of an embryo. The parafasicular and central lateral nuclei appear to be a logical place to start. It is also conceivable that such a structure may be extremely small and may be buried in the hypothalamus rather than the thalamus (Fig. 2).
The thalamic neuron theory also proposes the acupuncture meridians to be equivalent to neuronal chains within the homunculus. It has been pointed out by some that the meridians actually resemble the embryonic cleavage planes. So this is in further agreement with the hypothesis that the primitive nucleus which contains the homunculus is in reality the embodiment of the master plan for embryological development. The implications here are far reaching. It has been long established that denervation will cause muscle to atrophy. Limb regeneration in certain lower vertebrates is dependent on intact nervous tissue. Transplanting a nerve from a fast contracting muscle to a slow contracting muscle can convert the latter into a fast contracting muscle and vice versa. The trophic effects exerted on the entire body by the nervous system may be much more extensive than at present imagined. Suppose the primordial nucleus continues to control and regulate through direct and indirect connections the later additions of the brain, which in turn control and regulate other physiological processes, then it is not unthinkable that stimulation of strategic foci in the phylogenetically senior areas of the brain can bring about remarkable normalizing and hence therapeutic effects in many pathological states.
REFERENCES
-
Sunderland S. News and Nerve Injuries.
E & S Livingstone, Edinburgh, 1968.
-
Echlin F. Owens FM, Wells WL. Observations
on "major" and "minor" causalgia. Arch Neurol Psychiatry 62, 183, 1949
-
Berges PV. Myofascial pain syndromes.
Postgrad Med. 53, 161-168, 1973
-
Sola AE, Williams RL. Myofascial pain
syndromes. Neurology 6, 91-95, 1956
-
Priest JD, Jones HH, Nagel DA. Elbow
injuries in highly skilled tennis players. J Sports Med. 2, 137-149, 1974
-
Samberg HH. The trigger point syndrome.
GP. 35, 115-117, 1967
-
Frost EAM, Hsu CY. Neurophysiologic
pathways in acupuncture. Am J Acupuncture 3, 331-334, 1975
-
Chapter on meridian tendon, Ling Shu,
Yellow Emperor's Classic on Internal Medicine, 400 B.C. approximately.
-
Richardson DE. Thalamotomy for intractable
pain. Confin Neurol. 29, 139-145, 1967
-
Uematsu S. et al. Thalamotomy for alleviation
of intractable pain. Confin Neurol. 36, 88-96, 1974
-
Fairman D, Llavallol MA. Thalamic tractotomy
for the alleviation of intractable pain in cancer. Cancer 31, 700-707,
1973
-
Fairman D. Evaluation of results in
stereotactic thalamotomy for the treatment of intractable pain. Confin
Neurol. 27, 67-70, 1966
-
Fairman D. Stereotactic treatment for
the alleviation of intractable pain, reassessments and limitations. Confin
Neurol. 32, 341-344, 1970
-
Loeser JD. Neurosurgical relief of chronic
pain. Postgrad Med. 53, 115-119, 1973
-
Rosomoff HL. Neurosurgical control of
pain. Ann Rev Med. 20, 189-200, 1969
-
Loeser JD. Dorsal rhizotomy for the
relief of chronic pain. J Neuro Surg. 36, 745-750, 1972
-
Onofrio BM, Campa HK. Evaluation of
12 years experience. J Neuro Surg. 36, 751-755, 1972
-
Hassler R. "Afferent systems", Pain.
Williams and Wilkins, Baltimore, Maryland.
-
Delgado MR. Brain "pacer" fully blocks
stubborn pain. Med Tribune, April 24, 1974.
-
Kandel ER. Nerve cells and behavior.
Sci Amer. 233, 57-67, 1970
-
Chang Hsiang-Tung: Integrative action
of thalamus in the process of acupuncture for analgesia. Acta Scientifica
Sinica 1, 28, 1973; Am J Clin Med. 2, 1-39, 1974
|
|
